Patella dislocations are a very common orthopedic diagnosis and are mainly caused by internal damage to the medial patellofemoral complex. The medial patellofemoral complex is an important soft tissue restraint of the patellofemoral joint, consisting of the medial patellofemoral ligament (MPFL), the medial patellotibial ligament, and the vastus medialis muscle. Medical studies have demonstrated the importance of the MPFL in the lateral stabilization of the patella. Thus, when damage is sustained, the repair or reconstruction of the MPFL is instrumental in maintaining the normal motion of the patellofemoral joint.

Currently, a common technique for restoring the normal functions of the MPFL is through tendon reconstruction. Tendon reconstruction has consistently been able to improve patella stability and patient quality of life following injury. However, tendon reconstruction surgery require an autograft of tissue around the patient’s knee joint, which comes with additional risks of complications resulting in changes in joint mechanics and stride patterns. Another technique known as suture tape augmentation overcomes these risks; however, its efficacy in improving patella stability has yet to be determined.
Dr. Huang Yong from the Shenzhen Second People’s Hospital did a comparative study on the two techniques discussed above. Multiple anatomical specimens of knee joints were selected for this test, and for each test condition, three complete extension and flexion cycles were performed. The first cycle was used as a control group, and the average measurements from subsequent cycles were calculated for comparison. Six different levels of knee joint flexion were tested: 0°, 10°, 20°, 30°, 60° and 90°; the mean contact pressure (MP), peak contact pressure (PP), contact area (CA), patellar shift (PS), and patellar tilt (PT) was recorded for each trial.
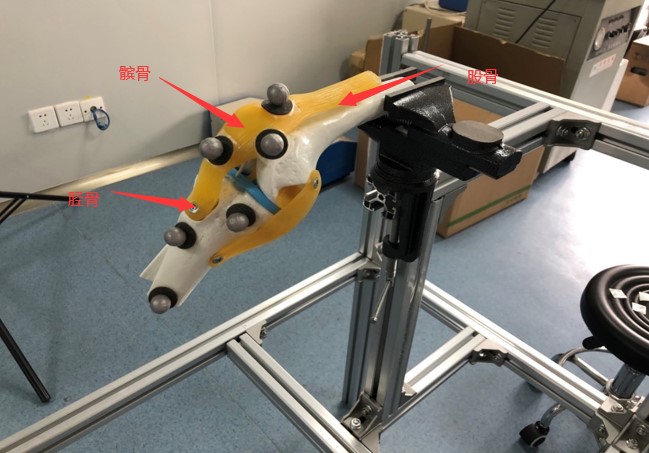
The NOKOV optical motion capture system was used to measure the patellar shift and patellar tilt throughout the experiment. In the experiment, the femur was horizontally stabilized, while the tibia was fixed to an articulated arm such that it could rotate freely. Reflective markers were attached to the surfaces of the femur, tibia, and patella. The quadriceps femoris and iliotibial band were each loaded with three different weights (2N, 5N, and 10N), and the subsequent patellar shift and patellar tilt were recorded for each repair technique. The figure below shows a simple demonstration of the experiment‘s design.

After all trials were completed, matched-pairs t-tests were conducted on knee joint specimen at different flexion angles to determine the differences between the efficacy of tendon reconstruction and suture band augmentation of the MPFL under different loads.